By
Liz Highleyman
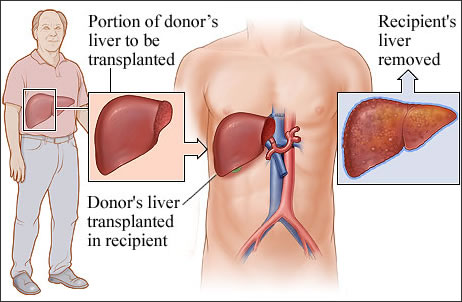
Liver
transplantation is currently the only treatment for highly
advanced liver damage due to chronic
hepatitis C virus (HCV) infection. But the virus almost
always re-infects the new liver, often leading to poor outcomes.
F.D.
Gordon and fellow investigators with the Phase 3b PROTECT study,
sponsored by Schering-Plough, evaluated the safety and efficacy
of 1.5 mcg/kg/week pegylated
interferon alfa-2b plus 400-1200 mg/day ribavirin for up
to 48 weeks in patients with recurrent HCV infection following
orthotopic liver transplantation.
The single-arm, open-label study enrolled 125 participants at
24 U.S. sites. Most (85%) were men, 81% were white, and most
had hard-to-treat HCV genotype 1 (84%) and high baseline HCV
viral load > 600,000 IU/mL (89%).
Results
 |
73
participants completed treatment and 52 discontinued therapy
early. |
 |
In
an intent-to-treat analysis, the overall SVR rate was 28.8%. |
 |
Genotype
1: 23.8%; |
 |
Genotypes
2 or 3: 55.0%. |
|
 |
Among
patients who completed therapy, however, the sustained response
rate was 54.5%. |
 |
Genotype
1: 50.5%; |
 |
Genotypes
2 or 3: 68.8%. |
|
 |
83.3%
of patients who achieved rapid virological response (RVR)
at week 4 went on to achieve SVR. |
 |
66.7%
of participants with complete early virological response
(EVR) at week 12 achieved SVR, compared to 36.1% with only
partial EVR. |
 |
The
overall relapse rate was 18.2% (19.4% for genotype 1, 15.4%
for genotypes 2 or 3). |
 |
Patients
who achieved SVR received a significantly higher mean ribavirin
dose than non-responders (10.4 vs 8.8 mg/kg/day, respectively). |
 |
55%
of participants required dose reductions and 30% discontinued
treatment due to adverse events. |
 |
26%
of patients experienced serious adverse events. |
 |
Reported
adverse events included anemia (74%), fatigue (71%), headaches
(62%), neutropenia (30%), insomnia (29%), depression (23%),
and anxiety (15%).
|
 |
Just
over half had severe anemia and a similar proportion had
severe neutropenia (low level of infection-fighting white
blood cells). |
 |
4
patients (3%) experienced rejection of the new liver.
|
Overall,
29% of post-orthotopic liver transplant patients receiving pegylated
interferon alfa-2b plus ribavirin achieved SVR, or 54.5% among
treatment completers, the study investigators concluded.
"End of treatment response was predictive of SVR, with
a relapse rate of 18%," they continued. "RVR and complete
EVR were also predictive of SVR and rejection rate was low."
They suggested that hematologic adverse events, or low blood
cell counts -- a common reason for early discontinuation --
"may be a modifiable barrier to treatment in this population."
Use of erythropoietin to manage anemia or growth factors to
manage neutropenia, for example, might allow more people to
stay on treatment.
Researcher affiliations: Transplantation, Lahey Clinic Medical
Center, Burlington, MA; Columbia University College of Physicians
& Surgeons, New York-Presbyterian Hospital, New York, NY;
Medicine, Indiana University, Indianapolis, IN; The Liver Institute
at Methodist Dallas Medical Center, Dallas, TX; Washington University,
St. Louis, MO; Division of Transplantation Medicine, Mayo Clinic,
Scottsdale, AZ; Henry Ford Hospital, Detroit, MI; Mount Sinai
Medical Center, New York, NY; Schering-Plough Research Institute,
Kenilworth, NJ.
5/4/10
Reference
FD Gordon, RS Brown, P Kwo, and others. Peginterferon alfa-2b
and ribavirin for hepatitis C recurrence post orthotopic liver
transplantation (OLT): final results from the PROTECT Study.
45th Annual Meeting of the European Association for the Study
of the Liver (EASL 2010). Vienna, Austria. April 14-18, 2010.
(Abstract).