Entecavir
(Baraclude) Improves Liver Function in Chronic Hepatitis B Patients
with Decompensated Cirrhosis
 |
 |
 |
 |
 |
 |
 |
| SUMMARY:
The antiviral drug entecavir
(Baraclude) worked as well in chronic hepatitis
B patients with decompensated liver disease as it
did in individuals with less severe liver damage,
according to a study published in the February
2010 Journal of Hepatology. Furthermore,
over 1 year, entecavir improved underlying liver function
in these patients with the most advanced disease.
|
|
 |
 |
 |
 |
 |
 |
 |
By
Liz Highleyman
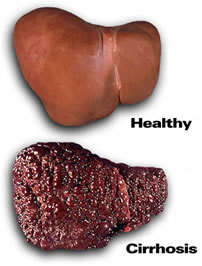 Over
years or decades, chronic hepatitis
B virus (HBV) infection can progress to advanced liver disease
including cirrhosis (scarring)
and hepatocellular carcinoma.
Compensated cirrhosis means the liver is heavily damaged but
can still carry out its normal functions; decompensated cirrhosis
occurs when the liver fails to perform properly.
Over
years or decades, chronic hepatitis
B virus (HBV) infection can progress to advanced liver disease
including cirrhosis (scarring)
and hepatocellular carcinoma.
Compensated cirrhosis means the liver is heavily damaged but
can still carry out its normal functions; decompensated cirrhosis
occurs when the liver fails to perform properly.
Several
antiviral agents are used to treat chronic hepatitis B, but
therapy can be risky in patients with decompensated cirrhosis.
However, this group also stands to benefit most from effective
treatment.
Ju Hyun Shim from the University of Ulsan College of Medicine
in Seoul and colleagues evaluated entecavir as first-line monotherapy
in a group of 70 Korean hepatitis B patients with decompensated
cirrhosis who started treatment with 0.5 g/day entecavir between
January 2007 and March 2008.
None
of the patients had received prior therapy using other antiviral
agent or interferon. Participants had HBV DNA viral load levels
of at least 4 log copies/mL at baseline. None had evidence of
hepatocellular carcinoma the time of treatment initiation and
none had undergone prior liver transplantation; individuals
with HIV or hepatitis
C coinfection were excluded.
Liver cirrhosis was diagnosed based on clinical, radiological,
or histological (biopsy) assessments. Decompensated disease
was defined as a Child-Turcotte-Pugh (CTP) score of 7 or higher
(class B and C) or the presence of portal hypertension complications
such as ascites (abdominal fluid accumulation), bleeding varices,
or hepatic encephalopathy (brain impairment).
The investigators looked at clinical outcomes among all 70 decompensated
patients using an intent-to-treat analysis. They also compared
responses in 55 decompensated patients who received entecavir
for at least 12 months and 144 patients with compensated liver
disease. In both groups, about one-third were women and approximately
half were hepatitis B "e" antigen (HBeAg) positive,
but the decompensated patients were slightly older on average
(53 vs 47 years).
The decompensated and compensated groups were evaluated every
3-6 months with tests for liver function, prothrombin time (a
measure of blood clotting), HBeAg, HBe antibodies, and HBV DNA
levels.
Results
 |
6
decompensated patients (8.6%) died during follow-up (all
due to liver failure within 6 months of starting entecavir);
3 patients (4.3%) underwent liver transplants 3-4 months
after starting entecavir; and 6 patients (8.6%) were lost
to follow-up before the 12-month evaluation, but were still
alive. |
 |
Among
the 70 decompensated cirrhosis, the 1-year cumulative transplant-free
survival rate was 87.1%, falling to 83.0% at 2 years. |
 |
After
6 months on entecavir, only 1 decompensated patient died
of a liver-related cause (uncontrollable bleeding varices)
and no additional patients received liver transplants. |
 |
4
of the 70 decompensated patients developed hepatocellular
carcinoma during follow-up, for a cumulative 24-month incidence
of 6.9%. |
 |
Entecavir
led to a progressive decrease in HBV DNA levels during treatment
(-5.52 log copies/mL at 6 months, -6.76 log copies/mL at
12 months). |
 |
The
overall 1-year cumulative rate of undetectable HBV DNA among
all 199 patients was 84.4% (81.3% in the compensated group
vs 92.7% in the decompensated group, not a statistically
significant difference; P = 0.099). |
 |
Among
the 70 decompensated patients in an intent-to-treat analysis,
the 1-year cumulative rate of undetectable HBV DNA was 92.3%. |
 |
Within
this same group the rate of HBeAg loss was 54.0%.
" Among the decompensated patients, entecavir treatment
for 12 months led to improvements in: |
| |
 |
CTP
score (8.1 pre-treatment vs 6.6 post-treatment); |
 |
MELD
liver function score (11.1 vs 8.8, respectively); |
 |
Mean
serum albumin (2.8 vs 3.2 g/dL, respectively); |
 |
Total
bilirubin (3.0 vs 1.9 mg/dL, respectively); |
 |
Prothrombin
time (16.3 vs 13.9 seconds, respectively). |
|
 |
65.5%
of decompensated patients reached CTP class A (the least
severe level) and 49.1% showed a CTP score improvement of
more than 2 points. |
 |
Rates
of undetectable HBV DNA, HBeAg seroconversion or loss, and
ALT normalization at 1 year were similar in the decompensated
and compensated groups. |
 |
Pre-treatment
HBeAg seropositivity was the only significant negative predictor
of HBV DNA clearance during entecavir therapy (hazard ratio
0.514; P < 0.001). |
Based
on these findings, the study authors wrote, "One-year initial
entecavir therapy was similarly effective in both compensated
and decompensated liver disease HBV patients. In addition, it
improved underlying liver function in decompensated patients."
"The results presented here clearly confirm that first-line
entecavir monotherapy provides comparable overall antiviral
benefits in HBV-infected patients with decompensated cirrhosis
as has been shown in patients with chronic hepatitis or compensated
cirrhosis, regardless of HBeAg serostatus," they elaborated
in their discussion.
In conclusion, they wrote, "the present study provides
evidence that 1 year of initial entecavir treatment is comparably
efficacious in arresting HBV replication and clearing HBeAg
in HBV-infected patients with either compensated or decompensated
liver disease."
"In addition, entecavir markedly improved the underlying
hepatic reserve in decompensated cirrhotic patients, mostly
within 6 months of treatment," they continued. "Thus,
our findings may establish a rationale for the use of entecavir
as a first-line monotherapeutic agent in these patients."
In
an accompanying editorial, Robert Fontana from the University
of Michigan Medical Center at Ann Arbor wrote that Shim and
colleagues "convincingly show that entecavir at a dose
of 0.5 mg per day is effective in treating naive decompensated
HBV patients with nearly 90% achieving undetectable HBV DNA
at month 12. In addition, suppression of HBV DNA was maintained
during follow-up with no instances of viral rebound or entecavir-resistant
HBV identified."
However, he continued, "the authors also note that not
all decompensated patients improved with entecavir therapy,"
with 12 participants (22%) showing no change in CTP score at
1 year and 4 experiencing worsening CTP scores. "Whether
this 'aggravation' was related to entecavir treatment or progression
of their underlying liver disease is unclear," he wrote.
All approved oral HBV drugs carry a "black box" warning
about their potential to cause mitochondrial toxicity, which
can manifest as lactic acidosis, myopathy (muscle damage), neuropathy
(nerve damage), or hepatotoxicity (liver toxicity). Laboratory
studies suggest that entecavir is less likely to cause mitochondrial
damage than other anti-HBV agents, but
it has been reported.
Despite this caveat, Fontana concluded, "the study of Shim
et al. and others...are bright stars in the horizon for the
management of decompensated HBV cirrhosis. The aggregate efficacy
and safety data now support the use of entecavir as a first
line treatment option for nucleos(t)ide naive patients with
decompensated HBV cirrhosis. However, continued follow-up from
these ongoing studies including long-term efficacy, safety,
and resistance data are needed."
Department of Internal Medicine, Asan Medical Center, University
of Ulsan College of Medicine, Seoul, Republic of Korea.
2/9/10
References
JH
Shim, HC Lee, KM Kim, and others. Efficacy of entecavir in treatment-naive
patients with hepatitis B virus-related decompensated cirrhosis.
Journal of Hepatology 52(2): 176-182 (Abstract).
February 2010.
RJ
Fontana. Entecavir in decompensated HBV cirrhosis: The future
is looking brighter (editorial). Journal of Hepatology Hepatology
52(2): 147-149 (Free
full text). February 2010.
