Effectiveness
of Statins among HIV Positive People on Antiretroviral Therapy
 |
 |
 |
 |
 |
 |
 |
| SUMMARY:
Atorvastatin (Lipitor) and rosuvastatin (Crestor)
may be the best choices for HIV positive people
who need a statin drug to control elevated cholesterol,
according to a study report in the December
28, 2010 advance online edition of Clinical Infectious
Diseases. Researchers found that these 2
medications produced greater decreases in total
and LDL cholesterol, with about the same degree
of toxicity as pravastatin (Pravachol). |
|
 |
 |
 |
 |
 |
 |
 |
By
Liz Highleyman
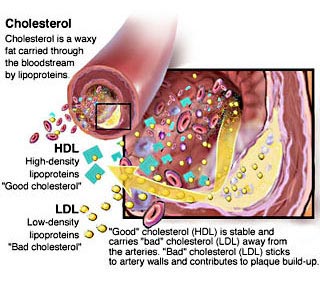
 Abnormal
blood fat levels, or dyslipidemia, are common among people
with HIV and are associated with certain antiretroviral
drugs. Lifestyle changes such as improved diet and more
exercise can help lower harmful low-density lipoprotein (LDL)
"bad" cholesterol and raise protective high-density
lipoprotein (HDL) "good" cholesterol, but such measures
may not be adequate, necessitating use of statins (also known
as HMG CoA reductase inhibitors). Abnormal
blood fat levels, or dyslipidemia, are common among people
with HIV and are associated with certain antiretroviral
drugs. Lifestyle changes such as improved diet and more
exercise can help lower harmful low-density lipoprotein (LDL)
"bad" cholesterol and raise protective high-density
lipoprotein (HDL) "good" cholesterol, but such measures
may not be adequate, necessitating use of statins (also known
as HMG CoA reductase inhibitors).
In an effort to learn more about the comparative effectiveness
of this class of drugs in HIV positive people, researchers
from the University of Washington and University of Alabama
compared the effectiveness and toxicity of different statins
among HIV patients in clinical care.
This retrospective analysis included 700 HIV positive individuals
starting their first treatment with statins at 2 large HIV
clinics between 2000 and 2008. Most (86%) were men, the average
age was 43 years, and the mean nadir (lowest-ever) CD4 T-cell
count was 182 cells/mm3.
Researchers looked at changes in blood lipid levels during
statin therapy, whether patients achieved National Cholesterol
Education Program (NCEP) goals for LDL and HDL levels, and
drug-related adverse events or toxicities.
Results
 |
The
most commonly prescribed statins were: |
| |
 |
Atorvastatin:
303 patients, 43%; |
 |
Pravastatin:
280 patients, 40%; |
 |
Rosuvastatin:
95 patients, 14%; |
 |
Simvastatin
(Zocor): 14 patients, 2%; |
 |
Fluvastatin
(Lescol): 5 patients, <1%; |
 |
Lovastatin
(Mevacor): 3 patients, <1%. |
|
 |
1
year after starting statin therapy, patients who received
atorvastatin or rosuvastatin experienced significantly
larger blood lipid decreases compared with those taking
pravastatin: |
| |
 |
Total
cholesterol: 39, 43, and 25 mg/dL, respectively; |
 |
LDL
cholesterol: 26, 23, and 12 mg/dL, respectively; |
 |
Non-HDL
cholesterol: 39, 47, and 26 mg/dL, respectively; |
 |
Triglycerides:
60, 83, and 24 mg/dL, respectively. |
|
 |
People
who used atorvastatin or rosuvastatin were also significantly
more likely to reach NCEP goals for LDL than those taking
pravastatin (odds ratio [OR] 2.1, or about twice as likely). |
 |
The
likelihood of reaching NCEP goals for non-HDL was higher
for rosuvastatin, but not for atorvastatin, relative to
pravastatin (OR 2.3 and 1.5, respectively). |
 |
Toxicity
rates were similar for all 3 statins: |
| |
 |
7.3%
for atorvastatin; |
 |
6.1%
for pravastatin; |
 |
5.3%
for rosuvastatin. |
|
 |
Among
the 44 patients who experienced toxicities, 15 -- or just
2.2% of all study participants -- had potentially serious
adverse events. |
 |
Elevated
creatine phosphokinase (CPK), with or without a decline
in kidney function, was the most common potentially serious
toxicity, followed by elevated liver enzymes. |
 Based
on these data, the study authors concluded, "Our findings
suggest that atorvastatin and rosuvastatin are preferable
to pravastatin for treatment of HIV-infected patients with
dyslipidemia, due to greater declines in total cholesterol,
LDL [cholesterol], and non-HDL [cholesterol], with similar
lower toxicity rates." Based
on these data, the study authors concluded, "Our findings
suggest that atorvastatin and rosuvastatin are preferable
to pravastatin for treatment of HIV-infected patients with
dyslipidemia, due to greater declines in total cholesterol,
LDL [cholesterol], and non-HDL [cholesterol], with similar
lower toxicity rates."
"Results
from studies of the effectiveness and toxicity of statins
among HIV-infected individuals may differ from results for
the general population for several reasons," the researchers
explained in their discussion. "The patterns of dyslipidemia
commonly seen among HIV-infected individuals differ from those
in persons without HIV infection and may be less responsive
to treatment. Second, drug interactions between statins and
antiretroviral medications may impact the metabolism, effectiveness,
and toxicity risk associated with particular statins."
Guidelines
from the Infectious Disease Society of America and the Adult
AIDS Clinical Trials Group recommend atorvastatin or pravastatin
for HIV positive people -- in part because these drugs were
thought to be less likely to interact with antiretroviral
drugs metabolized by the cytochrome P450 3A4 enzyme -- but
the new findings "suggest that the lipid-lowering effectiveness
of pravastatin was significantly less than that of rosuvastatin
or atorvastatin."
"We
found a nonsignificant increase in HDL [cholesterol] levels
at 12 months among those receiving rosuvastatin," they
added. "HDL [cholesterol] may increase as much as 10%
with rosuvastatin among those without HIV. Our results are
consistent with the idea that combined (mixed) dyslipidemia
in HIV-infected patients may be more difficult to treat and
thus raises the question of whether combination therapy with
additional lipid-lowering agents may be needed."
Investigator affiliations: Department of Medicine, University
of Washington, Seattle, WA; Department of Medicine, University
of Alabama at Birmingham, Birmingham, AL.
1/11/11
Reference
S Singh, JH Willig, MJ Mugavero, and others. Comparative Effectiveness
and Toxicity of Statins Among HIV-Infected Patients. Clinical
Infectious Diseases (Free
full text). December 28, 2010 (Epub ahead of print).
|
